Abstract
Background: Outcome after haploidentical (Haplo) hematopoietic cell transplantation (HCT) is encouraging and has become alternative option to treat patients with high-risk hematological malignancies without human leukocyte antigen (HLA) matched donor. Currently, ex-vivo T-cell depletion (TCD) and unmanipulated graft with post-transplant cyclophosphamide (PTCy) remain the most commonly employed graft-versus-host disease (GVHD) prophylaxis strategies in patients receiving Haplo-HCT. The aim of this study is to compare the clinical outcome of adult patients with hematological malignancies receiving Haplo-HCT using these two different GVHD prophylaxis strategies.
Methods: We analysed 170 adults’ patients receiving haploidentical peripheral blood stem cell transplant for various hematological malignancies between Jan 2011 and July 2022, following myeloablative (MAC, n=21) or reduced intensity conditioning (RIC, N=149) regimen. 100 patients received Haplo-HCT with selective ex-vivo T cell (TCRαβ and CD45RA+) depleted grafts for GVHD prophylaxis (Haplo-TCD) (Koh LP et al. ASH 2018), whereas 70 patients received unmanipulated, T-cell-replete graft followed by PTCy (Haplo-PTCy), in combination with tacrolimus and mycophenolate mofetil for GVHD prophylaxis.
Results: Median time to neutrophil recovery was 12 days (range, 8-25) and 18 days (range 13-29) for patients receiving Haplo-TCD and Haplo-PTCY, respectively (p<0.001). Primary graft failure was seen in 1 patient in each of the 2 groups. Cumulative incidence (C.I.) of non-relapse mortality (NRM) (22% vs 25%; p=0.508), relapse (22% vs 26%; p=0.561), day 180 grade 2-4 acute GVHD (aGVHD) (35% vs 33%; p=0.539), day 180 grade 3-4 aGVHD (11% vs 3%; p=0.508) were not significantly different between the Haplo-TCD and Haplo-PTCy cohorts. However, C.I. of chronic GVHD (cGVHD) at 2 years was significantly lower in Haplo-TCD as compared with Haplo-PTCy (4% vs 26%, P<0.001).
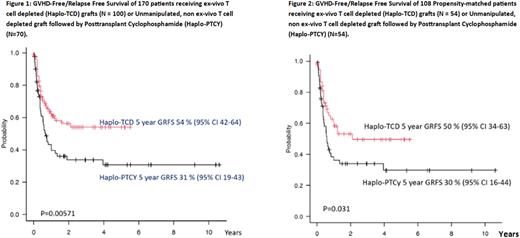
At a median follow up of 19.7 months (range 0.3- 67.1) in surviving patients, the 2-year overall (OS), event-free (EFS), and GVHD-free/relapse-free (GRFS) survival were 62% vs 49% (p=0.083), 56% vs 42% (p=0.309) and 54% vs 31% (p=0.006) for Haplo-TCD and Haplo-PTCy, respectively.
Multivariable analysis showed that disease risk index (DRI), HCT-Comorbidity Index (HCT-CI) and GVHD prophylaxis strategies were independent risk factors for OS, EFS and GRFS. In contrast, NRM was only influenced by HCT-CI (p=0.007), whereas relapse was only influenced by DRI (p=0.0001). Notably, Haplo-TCD was associated with significantly lower risk of cGVHD in multivariable analysis (HR 0.14; 95% CI 0.04-0.15; p=0.0011), and this translates into significantly more favorable GRFS as compared to Haplo-PTCy (Figure 1).
We performed propensity scoring for matching and identified 54 patients in each cohort. With propensity score matching, the use haplo-TCD retained its significant prognostic impact with lower risk of cGVHD (HR 0.08; 95% CI 1-62; p=0.016), and resulting in more favorable 5 years GRFS (50% vs 30%; p=0.03) as compared to Haplo-PTCy recipients (Figure 2). There was no significant difference in OS, EFS, CI of relapse, NRM, acute GVHD 2-4 and 3-4 between the 2 groups.
Conclusions: As compared to unmanipulated graft and PTCy, Haplo-HCT using ex-vivo TCRαβ and CD45RA+ depleted graft resulted in comparable outcome, with the additional advantage of earlier neutrophil engraftment, lower risk of cGVHD and more favorable GRFS. The difference in the post-transplant outcome with these two GVHD prophylaxis strategies warrants further investigation and confirmation in prospective controlled trials.
Disclosures
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal